Despite advances in cancer screening, detection, diagnosis, and management, many patients face challenges in accessing patient-centered, high-quality care in the United States due to systemic, cultural, and individual barriers. One evidence-based method for overcoming these obstacles is patient navigation, which aims to improve cancer outcomes and equity by reducing barriers and facilitating patients’ access to care.
In late 2023, the President’s Cancer Panel (the Panel) held a series of meetings on opportunities to enhance patient navigation with technology to improve equity in cancer care. The Panel concluded that health technology provides both new solutions and new challenges and that healthcare organizations, policy, and research must keep pace with technology’s rapid advancement and adoption in order to minimize cancer disparities and improve health outcomes for all.
Part I. Achieving Equity in Cancer Care: The Need for Navigation and the Promise of Technology
The burden of cancer does not fall equally across all segments of the U.S. population. Some demographic groups—particularly people of color; those living in rural areas; those with limited educational attainment or economic resources; lesbian, gay, bisexual, and transgender people; and those with disabilities—experience disproportionate rates of poor health and worse outcomes. Yet despite the evidence supporting its effectiveness in improving equity, patient navigation does not reach all patients who would benefit from it. Technological tools present one possible path to filling these gaps. Technology also has the potential to streamline cancer patient navigation and improve outcomes. The barriers to and risks of using technology to enhance cancer patient navigation are complex and are outlined in more detail in the priority area descriptions below.
Part II. Taking Action to Improve Equity with Technology-Supported Navigation
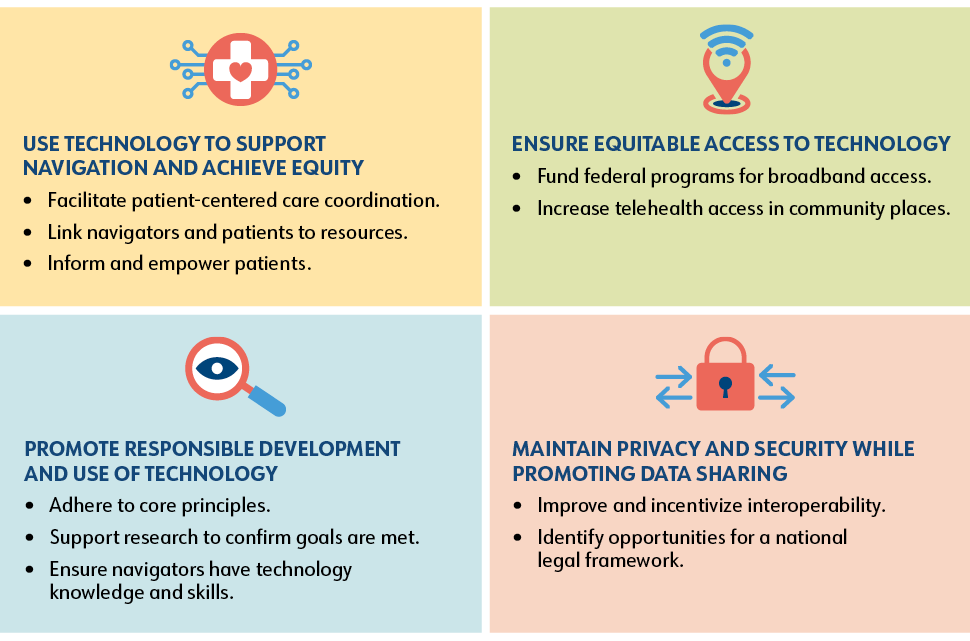
In this report, the Panel identifies four priorities and related recommendations regarding the development and use of technology for cancer patient navigation. Implementation of these recommendations should align with two foundational values: first, that technology should be used to augment, not replace, human interaction; and second, that access to or use of technology should not be a requirement for accessing high-quality cancer care and patient navigation.
Priority 1: Use Technology to Support Navigation Activities to Achieve Equitable Outcomes for People with Cancer
Navigation programs that spend more direct time with patients or with care team members on behalf of patients (as opposed to working in electronic health records [EHRs]) are more effective at improving access to timely care. Technology can help automate certain aspects of navigation and/or increase the efficiency of navigation processes so that care teams, including navigators, can spend more of their time caring for and interacting with patients.
Recommendation 1.1: Develop and implement tools that facilitate efficient, patient-centered coordination of cancer care.
Technology can help healthcare organizations address both systems and individual barriers to the delivery of timely, high-quality care. EHR vendors and healthcare organizations should assess the choice architecture of their EHR systems and implement and evaluate changes to improve workflow and delivery of care. Automatic referrals to appropriate providers and prompts for follow-up with patients who miss or are behind on recommended care could help ensure that no patient falls through the cracks. Technology in the form of automated tools embedded within EHRs could help more efficiently identify cancer patients who would benefit most from additional resources and services and ensure that those connections are made. Healthcare organizations should invest in and implement these tools and ensure that patients in need are referred to navigation services.
Recommendation 1.2: Develop and implement technologies to help navigators connect cancer patients with organizational and local resources.
Navigators are skilled at determining patients’ needs and how to meet them, yet this knowledge is often not shared in any centralized way. Healthcare organizations should establish navigator resource dashboards within EHR systems that allow navigators to link patients with resources that address their unique clinical and social needs. These dashboards should include a living and searchable database of institutional and local resources. This type of tool could significantly reduce administrative burden and streamline referrals, allowing navigators to spend more time directly supporting patients.
Recommendation 1.3: Develop and implement tools that provide vetted, personalized cancer-related information for patients and caregivers.
Patients should be able to easily conduct targeted searches and find results relevant to their specific diagnosis, treatment plan, and circumstances. This could be achieved through the creation of vetted search platforms; such tools would be even more powerful and precise if they were integrated with a patient’s own EHR data. Technology can also link patients with resources to meet nonclinical needs that arise over the course of their cancer diagnosis and treatment. Technology developers, advocacy organizations, and research funding organizations should invest in technology tools—such as patient-facing apps and decision support tools—that empower patients to navigate their cancer journey.
Priority 2: Ensure Equitable Patient Access to Technology That Supports Cancer Navigation
The communities most likely to experience health disparities are often also the ones with the least access to technology, including devices and broadband internet. These disparities occur at both the individual and collective levels and can limit patients’ access to care. The government approach to filling these gaps is complex and dispersed across numerous agencies and programs at the state and federal levels.
Recommendation 2.1: Provide sustainable funding for federal programs that facilitate access to broadband internet.
Ensuring equitable access to broadband internet will require both short-term and long-term funding mechanisms. The Panel has identified two actions to support this goal.
The Federal Communications Commission’s (FCC’s) Affordable Connectivity Program (ACP) provided crucial financial support to help households afford internet access, but funding for this program concluded in May 2024. Bipartisan efforts to renew the program have stalled, leaving millions of Americans with limited or no digital access to healthcare, work, school, and benefits. The Panel recommends that Congress and the President renew funding for the ACP, with the understanding that a longer-term mechanism will be required to provide ongoing funds.
The Universal Service Fund, also overseen by the FCC, enhances telecommunication access in low-income areas and aims to deliver service where it is needed most. Digital inclusion experts and the bipartisan Universal Service Fund Working Group in Congress are advocating for the modernization of this program to reflect the ways Americans use telecommunications today. The Panel urges continued work by the Universal Service Fund Working Group and recommends that reformation of the Fund include ongoing support for equitable broadband internet access through the ACP as well as sustainable funding for existing programs.
Recommendation 2.2: Increase patient access to devices and private space through community sites to facilitate access to telehealth appointments.
Patients need internet-connected devices and private, secure settings to comfortably and effectively access telehealth appointments, patient portals, and health information. A practical and relatively low-lift solution to this need is to create dedicated telehealth spaces within public places in the community. The Panel encourages continued support of telehealth access efforts in public libraries and other community settings, including through local, state, and federal funding. States and territories should make telehealth access a priority as they implement their Broadband Equity, Access, and Deployment (BEAD) Program plans in the coming years.
Priority 3: Promote Responsible Development and Use of Technology to Support Navigation
Technology does not automatically lead to increased efficiency or improved outcomes. Poorly designed and implemented health technology solutions can result in frustration, wasted resources, diminished trust, and even serious harm through medical errors or exacerbation of health disparities. Consensus-based frameworks are needed to ensure that the technologies used for cancer patient navigation are developed and used in ways that serve, protect, and build trust with patients. All frameworks and guidelines should adhere to a set of core principles, including:
- A people-first approach
- Equity
- User-centered design
- Effectiveness and validity
- Use of high-quality source data
- Transparency
- Privacy
- Interoperability
- Ongoing assessment and improvement
Recommendation 3.1: Adhere to core principles for responsible development and use of technologies that support cancer patient navigation.
All organizations that develop and use technology for cancer patient navigation should adhere to the core principles for navigation technology and use to ensure optimal benefit and return on investment. Organizations that purchase or fund development of technology for cancer patient navigation must take the lead in ensuring that technology is responsibly developed and implemented. Healthcare organizations should establish clear and binding expectations that all products purchased from or developed in partnership with third parties be responsibly developed, implemented, and assessed. Research funding organizations should include core principle requirements in the terms of award for any grant that involves development of a technology tool for patient navigation.
Recommendation 3.2: Support research to ensure that technology to support navigation achieves its goals.
Research is needed to explore new types of technology and new applications of existing technology that could be used to support navigation. Research funding organizations should provide funding for the development and testing of patient navigation technologies with a focus on tools that will address health disparities. Implementation research is also needed to determine the best ways to implement navigation-supporting technologies in real-world settings. The Agency for Healthcare Research and Quality (AHRQ) Digital Healthcare Research Program—which aims to produce and disseminate evidence about how the evolving digital healthcare ecosystem can best advance the quality, safety, and effectiveness of healthcare for patients and their families—is well suited to conduct this research. The Panel encourages AHRQ to assess technologies used by cancer patient navigators and care teams as well as those used by patients and caregivers.
Recommendation 3.3: Incorporate technology knowledge and skills into patient navigator training and core competencies.
The potential of technology-based tools for navigation can only be realized if navigation professionals understand and feel comfortable with using these tools. Navigator training programs should also incorporate learning objectives so that navigators understand how to use technology effectively and responsibly. As navigation technologies become more commonplace, digital skills should be included among oncology navigator core competencies such as those developed by the National Navigation Roundtable and Professional Oncology Navigation Task Force. Healthcare organizations must provide training for their navigators on any technology tool that is implemented within their system.
Priority 4: Maintain Privacy and Security While Facilitating Data Sharing to Support Cancer Patient Navigation
Effective cancer care delivery depends on the timely exchange of patient health data. At the same time, sensitive health information must be kept both private and secure. In an ideal world, data sharing would protect patient information without impeding its access and use by appropriate parties, including patients themselves. To create a seamless workflow for cancer patient navigation, patients and care teams—including navigators—need access to different types of data from different sources.
Recommendation 4.1: Improve and incentivize interoperability to enable portability of patient data across health IT platforms and systems in order to improve navigation.
The need for interoperability in health information technology has been a topic of discussion in the cancer community for some time. The federal government has made significant progress toward this aim, but there is significant work still to do. Continued progress toward interoperability and the seamless and secure exchange of health data to support cancer patient navigation and care will depend not only on regulations and guidance but also on cultural shifts within individual institutions and across the healthcare industry. The Panel acknowledges the many strides taken toward interoperability to date and encourages continued progress at the federal, industry, and health-system levels. Future efforts should include targeted investments to support participation of small practices in health information exchanges.
Recommendation 4.2: Evaluate existing privacy and security regulations and laws and identify opportunities for a national legal framework to protect patients while fostering technological innovation to support patient navigation.
The technological landscape has changed significantly since the Health Insurance Portability and Accountability Act of 1996 (HIPAA) and the 2009 Health Information Technology for Economic and Clinical Health (HITECH) Act were enacted; for example, more than half of U.S. adults report having used a mobile health application within the past 12 months. Although these apps generate, store, and use individuals’ health data, in most cases they are not considered covered entities or business associates under HIPAA and therefore are not subject to HIPAA standards of privacy and security.
There have been efforts to address these limitations and to protect the large and growing body of health data that falls outside the purview of HIPAA, and the federal government is working to address this gap from multiple perspectives. The Panel encourages continued discussion on this topic within and between all branches of the federal government. Mechanisms should be explored to protect patient data without obstructing data sharing and integration that support cancer care and research. The Panel recommends commissioning the National Academies of Sciences, Engineering, and Medicine to evaluate the current regulatory landscape and provide guidance to legislators on next steps to improve policies to better serve patients.
Part III. Conclusions
Patient navigation has been proven to reduce cancer disparities—a critical problem facing the National Cancer Program—by addressing individual and systemic barriers to accessing timely and high-quality care. In this report, the Panel identifies ways technology could be used to enhance evidence-based patient navigation for people with cancer.
The Panel has defined four priority areas and provided recommendations in each area to promote effective and appropriate use of technology for cancer navigation. These recommendations should be implemented in alignment with the following principles: first, that technology should augment, not replace, people; second, that technology must be responsibly developed and used; and third, that technology should help achieve equity, not exacerbate disparities.