Disparities in Cancer Care Access and Outcomes
The burden of illness does not fall equally across all segments of the U.S. population. Some demographic groups—particularly people of color; those living in rural or remote areas; those with limited educational attainment or economic resources; lesbian, gay, bisexual, and transgender people; and those with disabilities—experience disproportionate rates of poor health and worse outcomes. Disparities such as these are evident in cancer. (1,2,3,4,5,6) Advances in cancer detection and treatment are not reaching these populations at the same rate as for those with greater socioeconomic privilege, resulting in higher rates of morbidity and mortality. Disabled women with breast cancer, for example, are less likely than nondisabled women to be offered standard treatment. (3) Black patients, people with lower education levels, and those living in rural areas also have higher cancer-related mortality rates than members of other groups. (1,7)
Improving Equity with Cancer Patient Navigation
Despite advances in cancer screening, detection, diagnosis, and management, many patients face challenges in accessing patient-centered, high-quality care in the United States due to systemic, cultural, and individual barriers. (1,7) Navigating the cancer care journey is burdensome for patients due to a complex and fragmented healthcare system, and many patients are left behind. Major issues include delays in care, unmet social support needs, financial toxicity, reactive symptom management, high acute care utilization, and misaligned end-of-life care. Each of these issues has a disproportionate impact on under-resourced communities and marginalized populations. (8)
Patient navigation is an evidence-based intervention that was developed specifically to address these inequities (Figure 1). Navigation can include one or more of a variety of services and activities such as coordinating multidisciplinary care across the cancer continuum, including referrals to clinical trials; identifying and addressing barriers to care; and providing health education. The aim of patient navigation is to reduce barriers and facilitate a patient’s access to care by providing needed support services throughout the cancer journey. Each person’s navigation needs are unique; some patients require very little to no intervention, while others may need more support.
The first patient navigation program in the United States was developed by former President’s Cancer Panel Chair Dr. Harold Freeman in 1990. (9) Dr. Freeman’s program focused on using navigation to increase the uptake of cancer screening and early detection in his Harlem, New York, community. The program’s success inspired Dr. Freeman and others to expand the scope of patient navigation to encompass the entire cancer continuum. (10)
In the intervening decades, cancer patient navigation has consistently been demonstrated to improve outcomes; reduce disparities in cancer care; and lower costs for patients, healthcare organizations, and payors. Patients who receive navigation services have a shorter time to diagnosis and treatment, are more likely to complete their course of treatment, and report better understanding of their condition and the treatment process, as well as an overall higher quality of life. (9,10,11) However, patient navigation programs continue to face challenges (see Cancer Patient Navigation: Building Sustainable Programs).
The President’s Cancer Panel (the Panel) recognizes that navigation is invaluable for cancer patients and their families and endorses efforts to expand access to these services. The Panel is encouraged by progress being made in patient navigation and urges continued energy and advocacy in this area. Ideally, all patients with cancer would have access to comprehensive navigation services; however, this is not realistic in the current healthcare landscape. There are not enough resources or navigators to accomplish this even in high-resource settings, let alone in lower-resource settings in which navigation is even more critical. (11) Technology has the potential to support the professionals providing navigation services. If implemented thoughtfully, technological tools could extend the reach of limited navigation resources to more patients and help reach the goal of eliminating inequities in cancer care and outcomes.
There are many definitions of patient navigation. For the purposes of this report, the Panel is using the following definition:
Patient navigation is critical across the entire cancer continuum. Community-oriented outreach and support services, including those provided by community health workers, were identified as an important priority for cancer screening and follow-up in the 2022 Panel report Closing Gaps in Cancer Screening: Connecting People, Communities, and Systems to Improve Equity and Access. (12) The Panel reaffirms its recommendation that navigation services be available for cancer screening; however, the current report focuses on navigation after screening, from the time of diagnosis through treatment and beyond.
Figure 1. Patient Navigation
Potential for Technology-Supported Navigation
Nearly every aspect of daily life in the 21st century is shaped by technology. Computers, mobile devices, and the internet have revolutionized how people work, learn, play, interact, and care for their homes, their families, and themselves.
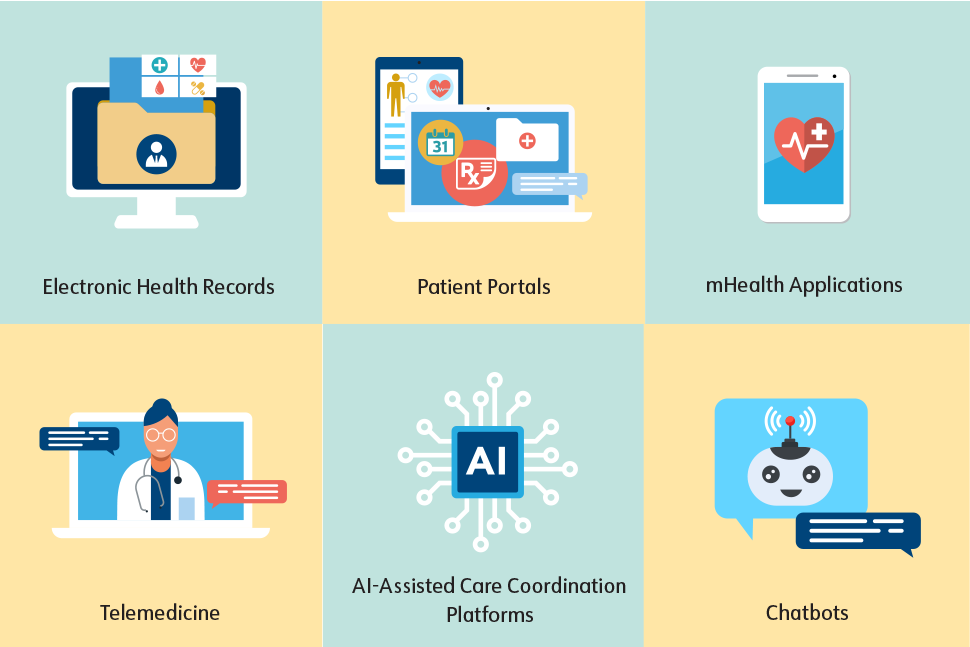
Technological tools—from electronic health records (EHRs) to telemedicine platforms—are now an integral part of healthcare. For the purposes of this report, the term “technology” refers to digital health technologies, a subset of tools that use computing platforms, connectivity, and software to support health and healthcare. Integrating technology into healthcare can result in increased health-related quality of life, fewer emergency department visits, reduced length of hospital stays, and reduced treatment-related toxicities. (19,20,21,22,23)
Technology also has the potential to streamline cancer patient navigation and improve outcomes (Figure 2). Today, healthcare providers, navigation professionals, and patients rely on a patchwork of technologies to support the cancer journey. Meeting attendees listed the health technologies most commonly used for navigation today as EHRs, digital screening tools, and patient portals. (24) Many patients also are seeking out information and tools outside of the healthcare system, including direct-to-consumer products designed to help patients manage and track their care. Technology-savvy patients may use smartwatches and other wearable devices to monitor vital signs and activity and/or download mobile applications (apps) to log their diet, exercise, symptoms, and medications or seek health advice. (25) Over the last few years, some health systems have begun to integrate various types of artificial intelligence (AI) into their workflows (see Artificial Intelligence to Support Patient Navigation: Opportunities and Concerns).
Technology applications will undoubtedly continue to expand into additional areas of health and healthcare in the coming years. Areas of opportunity for technology to support navigation of cancer patients and their families range from patient education to improved data collection and sharing, clinical trial matching, and more. The barriers to and risks of using technology to enhance cancer patient navigation are complex and are outlined in more detail in the priority area descriptions below. During the meeting series, stakeholders agreed that broad and successful implementation of digital solutions will require acknowledging and addressing barriers at the organizational, care team, and patient levels, including resource limitations; lack of payment models for training and tools, including mobile apps; technology fatigue; gaps in technological and health literacy; and limited interoperability among data platforms. (24)
In this report, the President’s Cancer Panel identifies four priorities and related recommendations to promote effective and responsible development and use of technology to support cancer patient navigation. Implementation of these recommendations will help extend the reach of patient navigation and improve the delivery of high-quality cancer care to all patients.