Objective 3: Ensure that federal programs and health IT tools support the oncology workforce as it delivers care.
Effective delivery of care across the cancer continuum is dependent on an engaged, productive workforce. Those involved in cancer care, like all health professionals, have had to adapt to massive changes in healthcare over the last several years, some of which have had a negative impact on the experience of providing care.[1] The rollout of EHR systems, in particular, has contributed to providers’ frustration and burnout.[2,3] Physician surveys have identified a number of ways in which EHRs significantly worsen professional satisfaction (see Sources of Providers’ Dissatisfaction with EHRs).[4-6] Among respondents to a 2015 American Society of Clinical Oncology survey of oncology practices, implementation and use of EHRs was the most commonly cited practice pressure, outranking payer pressures, staffing issues, and drug pricing.[7]
Sources of Providers’ Dissatisfaction with EHRs
- Time-consuming data entry
- Interfaces that do not match clinical workflow
- Difficulty finding important information
- Too many clicks required to complete common tasks
- Interference with face-to-face patient care
- Degradation of clinical documentation due to template-generated notes
- Inability to exchange information with other systems
- Too many automatic alerts and messages
- Costs of maintaining or changing systems
The transition to EHRs will not be reversed, and few physicians wish to return to paper-based medical records.[4] However, the significant challenges that have arisen during the initial rollout of EHRs should be addressed, and more work is needed to ensure interfaces are intuitive and aligned with care teams’ workflows.[3] Recent survey results suggest that progress is being made, as satisfaction with EHR systems has increased over the past few years among physicians in larger practices.[8] Many members of the healthcare delivery team already enjoy some advantages of EHRs—such as remote access to patient data, electronic prescribing, integrated graphing tools that display changes in disease markers over time, and improved communication with patients and other team members.[4,6,9,10] Additionally, most providers believe EHRs have potential to support improvements in both patient care and physician professional satisfaction.[4] Improvements in interoperability, as discussed in Objective 1, will further increase the utility of EHRs for providers by automating data flows between laboratories and offices/hospitals. Nevertheless, additional efforts are needed to ensure that federal programs and health IT tools support the oncology workforce as it strives to deliver the best possible care.
Action Item 3.1: Federal incentive programs should promote use of health IT to enhance provider delivery of high-quality, patient-centered care.
Widespread adoption of EHRs since the Health Information Technology for Economic and Clinical Health (HITECH) Act was passed in 2009 largely has been spurred by the Medicare and Medicaid EHR Incentive Programs, sometimes referred to as the “Meaningful Use” programs.[11] While the first stage of Meaningful Use, which focused on health IT adoption, generally is viewed as a success, providers increasingly have expressed concern about the second and third stages of the programs, citing inflexible assessment criteria, excessive documentation requirements, and focus on process-based tasks that are not directly related to—and sometimes interfere with—high-quality patient care.[12-14]
In January 2016, the Office of the National Coordinator for Health Information Technology (ONC) and the Centers for Medicare & Medicaid Services (CMS) publicly agreed that federal EHR incentive programs should be modified to allow providers flexibility in their use of health IT and measure success based on the quality of patient care and outcomes. Efforts currently are under way to modify the incentive program for those who give care to Medicare beneficiaries to reflect this focus (see Medicare Access and CHIP Reauthorization Act of 2015 ).[15] The President’s Cancer Panel supports efforts to reform federal incentive programs for EHR adoption and use. Regulations should not distract providers from patient care. Inherent in this, reporting requirements should be minimized.
Medicare Access and CHIP Reauthorization Act of 2015
A new Medicare EHR incentive program for clinicians currently is being developed under the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA). MACRA calls for a Merit-Based Incentive Payment System to measure eligible professionals based on quality, cost, technology use, and practice improvement rather than on the volume of services provided. Although the details of the program are still under development, the proposed rule calls for clinicians to report customizable measures that reflect how they use technology in their day-to-day practice, with a particular emphasis on interoperability and information exchange.
Sources: Centers for Medicare & Medicaid Services. The Merit-Based Incentive Payment System (MIPS) & Alternative Payment Models (APMs) [Internet]. Baltimore (MD): CMS; [cited 2016 Apr 25]. Available from: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Value-Based-Programs/MACRA-MIPS-and-APMs/MACRA-MIPS-and-APMs.html; U.S. Department of Health and Human Services. Administration takes first step to implement legislation modernizing how Medicare pays physicians for quality [News Release]. Washington (DC): DHHS; 2016 Apr 27. Available from: http://www.hhs.gov/about/news/2016/04/27/administration-takes-first-step-implement-legislation-modernizing-how-medicare-pays-physicians.html
Action Item 3.2: EHR vendors and healthcare organizations should employ human-centered design principles to ensure that EHR interfaces are intuitive and aligned with providers’ workflows.
Better medical record systems are needed that are dissociated from billing, intuitive and helpful, and allow physicians to be fully present with their patients.
Source: Zulman DM, Shah NH, Verghese A. Evolutionary pressures on the electronic health record: caring for complexity. JAMA. 2016;316(9):923-4. Available from: http://www.ncbi.nlm.nih.gov/pubmed/27532804
Many provider complaints about EHRs relate to poor usability and misalignment of interfaces with clinical workflows (see Sources of Providers’ Dissatisfaction with EHRs). This may be, in part, because systems were designed to optimize billing rather than clinical care.[16] Physicians report spending more time on clinical documentation following EHR adoption, which often results in less time for direct patient care, less patient engagement during visits, and more time spent on data entry outside of normal office hours.[3,4] Poor health IT usability also can undermine data quality and contribute to medical errors, a significant problem in the U.S. healthcare system.[17-19] In a review of extant EHR systems by the National Research Council, informatics experts reported that many of these systems failed to improve patient outcomes precisely because they failed to provide value-added support to healthcare delivery team members, patients, and their caregivers.[20]
Poor EHR usability is a significant barrier to deriving value from the sizable U.S. investment in health IT[18] and advancing connected health for cancer. EHR vendors and healthcare organizations should employ human-centered design processes during EHR development, as well as during deployment and testing phases, to ensure EHR interfaces are intuitive and aligned with providers’ workflows (see Human-Centered Design). Well-designed systems should reduce providers’ cognitive burden by automating routine tasks, minimizing the number of clicks it takes to complete an order, and adding point-of-need information for crucial decision making.[20]
Human-Centered Design
Human-centered design is a systematic approach to problem solving that is well suited for addressing complex issues at the intersection of people and technology. It encourages developers to repeatedly consider the context, emotions, needs, and desires of the intended users of a product and engages end users in the design process.
Source: Matheson GO, Pacione C, Shultz RK, Klugl M. Leveraging human-centered design in chronic disease prevention. Am J Prev Med. 2015;48(4):472-9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25700655
Action Item 3.3: Develop and test tools and interfaces, including apps, tailored to needs of the oncology workforce.
Innovative health IT tools and interfaces, including apps, could supplement traditional EHR interfaces in a number of ways, such as integrating and displaying data in meaningful ways, providing links to outside resources and knowledge bases, guiding delivery of evidence-based care, providing decision support, and facilitating communication among healthcare delivery team members. Tools that analyze large data sets and provide actionable recommendations based on the results—perhaps using artificial intelligence or machine learning[21]—will become more valuable, even essential, with the emergence of data-driven precision medicine (see Precision Medicine Initiative in Part 1 and Cancer Moonshot in Objective 5). These types of tools have potential to meet the specialized and diverse needs of the oncology workforce across the cancer continuum (Figure 2). To date, most tools developed have been for physicians, but other healthcare professionals who care for cancer patients—nurses, advanced practice providers, pharmacists, and others—also would benefit from customized tools.
Effective health IT tools can be developed by healthcare organizations and EHR vendors,[22] but the needs of the oncology workforce will be met most effectively if the full innovative capacity of the health IT community is harnessed. To enable this, EHR vendors and healthcare organizations must permit third-party health IT developers to safely and securely access their EHR data through application programming interfaces, or APIs (see Objective 1). Developers then will be able to develop a diverse suite of apps from which providers can choose based on their needs and preferences (Figure 6). Apps can be developed and modified more quickly than traditional EHR interfaces, allowing the marketplace to keep pace with advances in medical science and be responsive to providers’ feedback. Online resources—such as the app discovery site being developed by Boston Children’s Hospital with support from ONC[23]—can help providers find the apps and tools that best meet their needs.
Figure 6
API-Enabled Tools for Providers
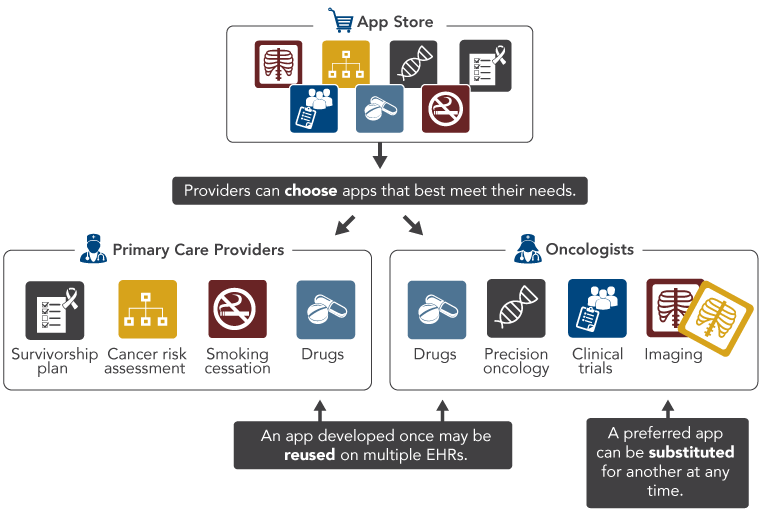
Adapted from Mandl K, Mandel J, Kohane I. Driving innovation in health systems through an apps-based information economy. Cell Systems. 2015;1(1):8-13. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26339683
Within the past few years, some EHR vendors have begun working collaboratively to expand API-mediated access to their systems.[24] ONC’s recent decision requiring health IT developers to include API functionality in their products and openly share API specifications in order to be certified will further increase third-party access to EHR systems.[25] API-based apps for providers are being developed and tested (see Precision Cancer Medicine App Helps Oncologists Use Genomic Information and Syapse Oncology), but more investment is needed in this area. The President’s Cancer Panel urges research funding organizations, such as the National Cancer Institute, to create initiatives to spur development by the health IT community of cancer-specific apps and tools for providers delivering cancer care across the continuum. The efficacy of tools and apps, particularly those designed to influence provider behavior, should be evaluated in order to identify the approaches that are most effective in a variety of settings and populations.
Precision Cancer Medicine App Helps Oncologists Use Genomic Information
Genomic data increasingly are informing treatment decisions for cancer patients and those at risk for cancer, but commercially available EHRs generally cannot display clinical genomic data in meaningful ways. The Precision Cancer Medicine (PCM) app was designed to present patients’ genomic test results to oncologists in real time as a component of clinical practice, as well as provide links to external knowledge bases that otherwise would be unavailable through the native EHR system. PCM was piloted at Vanderbilt University and integrated into that institution’s EHR system. However, because the app was developed based on an open-access API (Substitutable Medical Applications and Reusable Technology, or SMART) and uses the emerging HL7 Fast Healthcare Interoperability Resources standard, it could easily be deployed for other compatible EHR systems.
Sources: Mandel JC, Kreda DA, Mandl KD, Kohane IS, Ramoni RB. SMART on FHIR: a standards-based, interoperable apps platform for electronic health records. J Am Med Inform Assoc. 2016;23(5):899-908. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26911829; Warner JL, Rioth MJ, Mandl KD, Mandel JC, Kreda DA, Kohane IS, et al. SMART precision cancer medicine: a FHIR-based app to provide genomic information at the point of care. J Am Med Inform Assoc. 2016;23(4):701-10. Available from: http://www.ncbi.nlm.nih.gov/pubmed/27018265
Syapse Oncology
Syapse, a bioinformatics company founded in 2008, has developed a software platform that helps healthcare organizations systematize precision oncology. The software integrates with organizations’ EHRs and creates a unified, longitudinal view of each patient’s clinical, pathology, radiology, treatment, and molecular data. It also provides clinical decision support, suggesting targeted therapies based on patients’ genomic data, and permits providers to compare their patients with others within their organization based on tumor type, stage, genomic variants, and other factors. The Syapse platform also includes an automated clinical trial matching tool that identifies candidate patient-trial matches based on somatic mutation profile, clinical data, demographic information, or other criteria. In response to Vice President Biden’s Cancer Moonshot, Syapse also is working with multiple partners to make aggregate clinical data available for research through the Oncology Precision Network (OPeN).
Sources: Syapse. Home page [Internet]. Palo Alto (CA): Syapse; [cited 2016 Sep 9]. Available from: http://www.syapse.com/; Bin Han Ong M. Stanford, Intermountain, and Providence use Syapse platform to integrate their data. The Cancer Letter. 2016 Jun 24;42(25):1-6.
References
- Dyrbye LN, Shanafelt TD. Physician burnout: a potential threat to successful health care reform. JAMA. 2011;305(19):2009-10. Available from: http://www.ncbi.nlm.nih.gov/pubmed/21586718
- Babbott S, Manwell LB, Brown R, Montague E, Williams E, Schwartz M, et al. Electronic medical records and physician stress in primary care: results from the MEMO Study. J Am Med Inform Assoc. 2014;21(e1):e100-6. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24005796
- Wachter RM. The digital doctor. New York (NY): McGraw-Hill Education; 2015.
- Friedberg MW, Chen PG, Van Busum KR, Aunon FM, Pham C, Caloyeras JP, et al. Factors affecting physician professional satisfaction and their implications for patient care, health systems, and health policy. Santa Monica (CA): The RAND Corporation; 2013. Available from: http://www.rand.org/pubs/research_reports/RR439.html
- AmericanEHR, American Medical Association. Physicians use of EHR systems 2014. Naples (FL): AmericanEHR and AMA; 2014. Available from: http://www.americanehr.com/research/reports/Physicians-Use-of-EHR-Systems-2014.aspx
- Verdon DR. Physician outcry on EHR functionality, cost will shake the health information technology sector. Med Econ [Internet]. 2014 Feb 10 [cited 2016 Aug 3]. Available from: http://medicaleconomics.modernmedicine.com/medical-economics/content/tags/ehr/physician-outcry-ehr-functionality-cost-will-shake-health-informa
- American Society of Clinical Oncology. The state of cancer care in America, 2016: a report by the American Society of Clinical Oncology. J Oncol Pract. 2016;12(4):339-83. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26979926
- Black Book Market Research. Large physician groups eager to implement value-based reimbursement, finds 2016 Black Book EHR survey [Press Release]. Tampa (FL): Black Book Market Research; 2016 Jun 6. Available from: https://blackbookmarketresearch.newswire.com/news/large-physician-groups-eager-to-implement-value-based-reimbursement-11688129
- O'Malley AS, Draper K, Gourevitch R, Cross DA, Scholle SH. Electronic health records and support for primary care teamwork. J Am Med Inform Assoc. 2015;22(2):426-34. Available from: https://www.ncbi.nlm.nih.gov/pubmed/25627278
- Kruse CS, Mileski M, Alaytsev V, Carol E, Williams A. Adoption factors associated with electronic health record among long-term care facilities: a systematic review. BMJ Open. 2015;5(1):e006615. Available from: https://www.ncbi.nlm.nih.gov/pubmed/25631311
-
Centers for Medicare & Medicaid Services. Electronic health records (EHR) incentive programs [Internet]. Baltimore (MD): CMS; [updated 2016 Apr 14; cited 2016 May 6]. Available from: https://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/
index.html?redirect=/ehrincentiveprograms - Madara JL (Executive Vice President and CEO, American Medical Association). Letter to: Slavitt AM (Acting Administrator, Centers for Medicare & Medicaid Services) and DeSalvo KB (National Coordinator for Health Information Technology). 2015 Dec 15. Available from: https://download.ama-assn.org/resources/doc/washington/x-pub/meaningful-use-stage-3-comment-letter-15dec2015.pdf
- American Medical Association. Letter to: The Honorable Mitch McConnell and The Honorable Harry Reid (United States Senate). 2015 Nov 2. Available from: https://download.ama-assn.org/resources/doc/washington/x-pub/meaningful-use-sign-on-letter-senate-02nov2015.pdf
- American Medical Association. Letter to: The Honorable Paul Ryan and The Honorable Nancy Pelosi (United States House of Representatives). 2015 Nov 2. Available from: https://download.ama-assn.org/resources/doc/washington/x-pub/meaningful-use-sign-on-letter-house-02nov2015.pdf
- Centers for Medicare & Medicaid Services. The Merit-Based Incentive Payment System (MIPS) & Alternative Payment Models (APMs) [Internet]. Baltimore (MD): CMS; [cited 2016 Apr 25]. Available from: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Value-Based-Programs/MACRA-MIPS-and-APMs/MACRA-MIPS-and-APMs.html
- Zulman DM, Shah NH, Verghese A. Evolutionary pressures on the electronic health record: caring for complexity. JAMA. 2016;316(9):923-4. Available from: http://www.ncbi.nlm.nih.gov/pubmed/27532804
- Institute of Medicine. To err is human: building a safer health system. Kohn LT, Corrigan JM, Donaldson MS, editors. Washington (DC): National Academy Press; 2000. Available from: http://www.nap.edu/9728
- Riskin L, Koppel R, Riskin D. Re-examining health IT policy: what will it take to derive value from our investment? J Am Med Inform Assoc. 2015;22(2):459-64. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25326600
- Bowman S. Impact of electronic health record systems on information integrity: quality and safety implications. Perspect Health Inf Manag. 2013;10:1c. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24159271
- National Research Council. Computational technology for effective healthcare: immediate steps and strategic directions. Stead WW, Lin HS, editors. Washington (DC): The National Academies Press; 2009. Available from: http://www.nap.edu/12572
- Castaneda C, Nalley K, Mannion C, Bhattacharyya P, Blake P, Pecora A, et al. Clinical decision support systems for improving diagnostic accuracy and achieving precision medicine. J Clin Bioinforma. 2015;5:4. Available from: https://www.ncbi.nlm.nih.gov/pubmed/25834725
- Adsit RT, Fox BM, Tsiolis T, Ogland C, Simerson M, Vind LM, et al. Using the electronic health record to connect primary care patients to evidence-based telephonic tobacco quitline services: a closed-loop demonstration project. Transl Behav Med. 2014;4(3):324-32. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25264471
- DeSalvo K, Slavitt A. A foundation for discovering clinical health IT applications. Health IT Buzz [Internet]. 2016 Jun 1 [cited 2016 Aug 25]. Available from: https://www.healthit.gov/buzz-blog/from-the-onc-desk/foundation-discovering-clinical-health-applications/
- The Argonaut Project: project charter. 2015 Dec 4. Available from: http://mycourses.med.harvard.edu/ec_res/nt/6209858F-CDDD-4518-ADF8-F94DF98B5ECF/Argonaut_Project-12_Dec_2014-v2.pdf
- U.S. Department of Health and Human Services. 2015 Edition Health Information Technology (Health IT) Certification Criteria, 2015 Edition Base Electronic Health Record (EHR) Definition, and ONC Health IT Certification Program Modifications. Fed Regist. 2015 Oct 16;80(200):62602-759. Available from: https://www.federalregister.gov/articles/2015/10/16/2015-25597/2015-edition-health-information-technology-health-it-certification-criteria-2015-edition-base